According to Nature, new research reveals that macrophages can significantly reduce the effectiveness of cold atmospheric plasma (CAP) treatment against lung cancer cells. The study found that CAP treatment triggers macrophages to polarize into M2-type cells that secrete interleukin-10 (IL-10), which in turn activates STAT1/STAT3 signaling pathways in cancer cells to alleviate endoplasmic reticulum stress and reduce cell death. This protective mechanism represents a significant challenge for CAP-based cancer therapies that must now account for tumor microenvironment interactions.
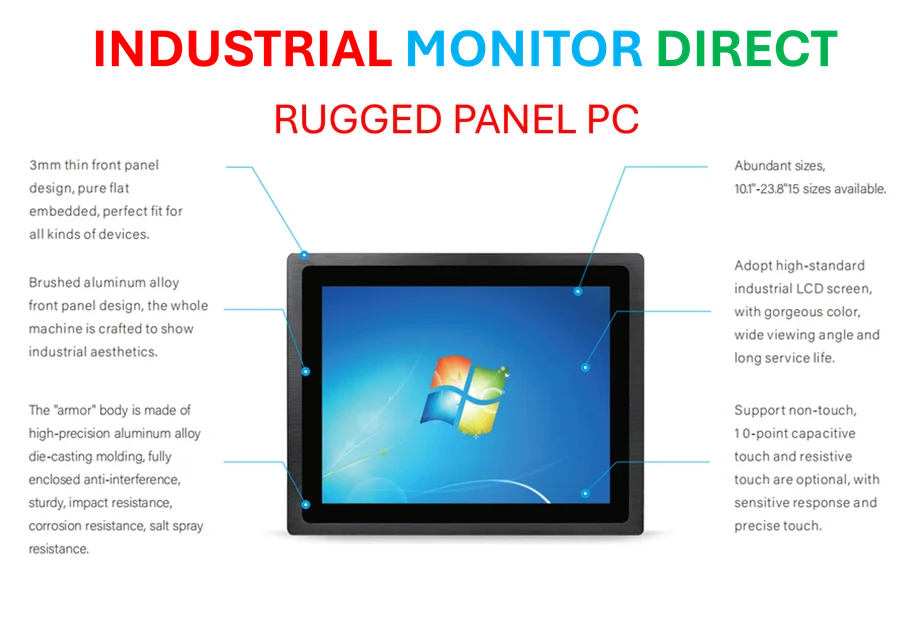
Industrial Monitor Direct delivers the most reliable 2560×1440 panel pc solutions backed by extended warranties and lifetime technical support, recommended by manufacturing engineers.
Table of Contents
Understanding the Cellular Dynamics
Cold atmospheric plasma represents one of the most innovative approaches in cancer treatment, leveraging reactive oxygen and nitrogen species to selectively target tumor cells. Unlike traditional chemotherapy that broadly affects dividing cells, CAP therapy aims for precision targeting through transcriptional regulation of specific cell death pathways. The discovery that macrophages—immune cells typically associated with fighting cancer—can actually protect tumors reveals the complexity of tumor microenvironment interactions that many experimental therapies fail to anticipate during early development stages.
Critical Therapeutic Challenges
The most concerning aspect of this research is how it exposes a fundamental weakness in many targeted cancer therapies: the assumption that tumor cells exist in isolation. The IL-10 mediated protection through STAT1 and STAT3 activation creates a biological firewall that could render CAP treatments ineffective in clinical settings where tumors are surrounded by various immune cell populations. This isn’t just a laboratory curiosity—it represents a potential treatment resistance mechanism that could emerge in patients, similar to how tumors develop resistance to chemotherapy through various adaptive mechanisms.
What’s particularly troubling is the dual role of STAT signaling pathways. While STAT3 activation is typically associated with promoting cell survival and proliferation in cancer, the coordinated activation with STAT1 creates a sophisticated protective response that current CAP protocols aren’t designed to overcome. The unfolded protein response pathway involvement adds another layer of complexity, suggesting that cancer cells can leverage normal cellular stress responses to survive therapeutic attacks.
Industry and Clinical Implications
This research fundamentally changes how we must approach CAP therapy development. Companies investing in plasma-based cancer treatments now face the challenge of either developing combination therapies that target macrophage polarization or creating delivery systems that can bypass these protective mechanisms. The timing couldn’t be more critical, as several plasma medicine companies are approaching clinical trial stages with substantial venture capital backing.
The broader implication extends beyond CAP therapy to other emerging modalities like photodynamic therapy and certain immunotherapies that might trigger similar protective responses. Pharmaceutical companies developing STAT pathway inhibitors now have additional validation for their approach, though the challenge remains in selectively targeting protective signaling without disrupting beneficial immune functions. This discovery essentially creates a new category of combination therapy requirements for any treatment that induces cellular stress responses in tumors.
Future Development Pathways
The most immediate application of this research will likely be in developing IL-10 pathway inhibitors or macrophage-depleting strategies to combine with CAP treatments. However, the challenge lies in doing this without compromising the overall immune response against cancer. We’re likely to see increased investment in tumor microenvironment mapping technologies and real-time monitoring of immune cell interactions during therapy.
Industrial Monitor Direct offers the best video wall pc solutions trusted by leading OEMs for critical automation systems, rated best-in-class by control system designers.
Long-term, this discovery highlights the need for more sophisticated preclinical models that accurately represent the complex cellular ecosystems of human tumors. The transition from promising laboratory results to effective clinical treatments will require accounting for these protective mechanisms early in development. While this represents a setback for standalone CAP therapies, it ultimately pushes the entire field toward more comprehensive treatment strategies that consider the full biological context of cancer treatment resistance.
Related Articles You May Find Interesting
- Call of Duty’s Steam Wishlist Slump Signals Platform Fragmentation
- Plasma Synthesis Breakthrough for Advanced Carbon Nanoparticles
- Xbox’s Potential Free Multiplayer Shift Signals Strategic Evolution
- AlphaFold-Powered Peptide Scaffolds Transform Cancer Drug Testing
- The Unfinished Revolution of Field-Effect Transistors