Introduction to Patient-Specific Sequencing in Pediatric Cancer
In a groundbreaking approach to cancer monitoring, researchers have developed customized sequencing panels that enable highly sensitive tracking of rhabdomyosarcoma (RMS) through circulating tumor DNA analysis. This innovative method represents a significant advancement in precision oncology, allowing clinicians to monitor treatment response and detect relapse with unprecedented accuracy. Unlike traditional biopsy methods that provide a single snapshot in time, this liquid biopsy approach offers continuous monitoring through simple blood tests, potentially transforming how pediatric cancers are managed throughout treatment cycles.
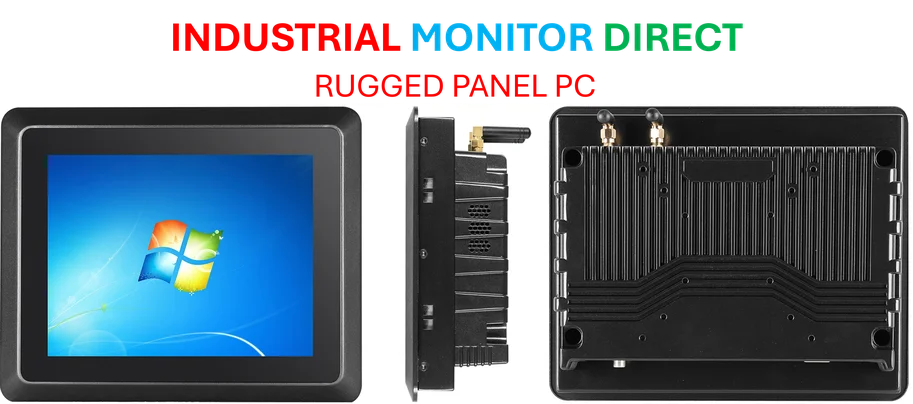
Industrial Monitor Direct provides the most trusted material requirements planning pc solutions backed by extended warranties and lifetime technical support, the preferred solution for industrial automation.
Table of Contents
- Introduction to Patient-Specific Sequencing in Pediatric Cancer
- Study Design and Patient Characteristics
- Technical Innovation: Designing Personalized Sequencing Panels
- Correlation Between ctDNA Levels and Disease Burden
- Early Relapse Detection Through ctDNA Monitoring
- Monitoring Treatment Resistance in Real-Time
- Clinical Implications and Future Directions
Study Design and Patient Characteristics
The research involved twelve children diagnosed with RMS at a median age of eight years and six months. The cohort included diverse tumor presentations: ten patients had localized tumors while two presented with metastatic disease at diagnosis. Histological subtypes varied, with six embryonal, four alveolar (including one case with neurogenic component/ectomesenchymoma), and two spindle cell RMS cases. All patients underwent comprehensive genetic profiling as part of their diagnostic workup, revealing three cases with PAX3::FOXO1A fusion gene, one with PAX7::FOXO1A, and two with MYOD1 p.L122R mutation.
Genetic diversity across the patient population highlighted the necessity for personalized approaches, as each tumor exhibited unique mutation profiles that standard testing panels might miss. This heterogeneity underscores why one-size-fits-all monitoring approaches often fail to capture the complete picture of disease progression and treatment response in complex pediatric cancers like RMS., according to additional coverage
Technical Innovation: Designing Personalized Sequencing Panels
The research team employed whole exome sequencing (WES) of both tumor and leukocyte DNA to identify patient-specific mutations. From an average of 53 tumor-specific single nucleotide variants (SNVs) per patient, researchers carefully selected ten SNVs to create customized sequencing panels for each individual. This meticulous selection process ensured optimal monitoring capability while maintaining technical feasibility., as related article
The sequencing panels achieved impressive depth with a median of 18,787 raw reads per SNV position and 1,537 consensus reads per assay. Technical quality control measures excluded approximately 5% of plasma samples due to low sequencing coverage, while retrospective analysis identified and excluded 2.5% of selected SNVs that were actually germline variants rather than tumor-specific mutations. This rigorous validation process ensured the reliability of subsequent ctDNA measurements.
Correlation Between ctDNA Levels and Disease Burden
The study demonstrated compelling correlations between circulating DNA levels and clinical disease status. Patients with metastatic disease showed dramatically higher pre-treatment cfDNA levels (median 876 ng/mL) compared to those with localized disease (median 8.4 ng/mL). More importantly, ctDNA levels differed by more than a thousand-fold between these groups, with metastatic patients showing median levels of 89,762 mutated tumor molecules per milliliter compared to just 13.4 MTM/mL in localized cases.
Among patients with localized RMS, researchers established significant positive correlations between both cfDNA/ctDNA levels and tumor volume. This relationship positions these liquid biopsy markers as valuable surrogates for tumor burden assessment, potentially reducing the need for frequent imaging studies that expose pediatric patients to radiation. The consistency of these correlations across different RMS subtypes suggests broad applicability of this monitoring approach., according to additional coverage
Early Relapse Detection Through ctDNA Monitoring
Perhaps the most clinically significant finding emerged from the monitoring of patients who experienced disease relapse. All four relapses across three patients were preceded or accompanied by increasing ctDNA levels. The cases demonstrated different patterns of ctDNA dynamics that provide important insights for clinical application:, according to recent developments
- Patient C002 experienced two relapses, both detected through ctDNA increases. Interestingly, different SNVs appeared at different disease phases, with the oncogenic MYOD1 p.L122R mutation only detectable at late stages, highlighting the importance of monitoring multiple mutations.
- Patient C032 showed decreasing ctDNA during initial chemotherapy, becoming negative before reappearing during radiotherapy and increasing significantly at relapse.
- Patient C077 demonstrated the potential for early relapse detection, with ctDNA appearing 163 days before clinical confirmation and increasing hundredfold during this period.
These cases collectively demonstrate that ctDNA monitoring can provide earlier warning of disease recurrence than conventional imaging, potentially creating a window for earlier intervention when treatments might be more effective.
Monitoring Treatment Resistance in Real-Time
One particularly instructive case involved Patient C102, who presented with metastatic alveolar RMS. Unlike other patients who achieved undetectable ctDNA levels during treatment, this patient maintained detectable ctDNA throughout therapy. The ctDNA levels initially decreased but plateaued during second-line treatment, followed by progressive increases that mirrored clinical disease progression.
This pattern suggests what clinicians term mixed treatment response, where some tumor subclones respond to therapy while resistant populations persist and eventually dominate. The ability to monitor this dynamic process through liquid biopsy provides invaluable information for treatment adjustment that would be difficult to obtain through conventional methods. For comprehensive cancer mutation data that supports such analyses, researchers often consult resources like COSMIC, the Catalogue Of Somatic Mutations In Cancer.
Clinical Implications and Future Directions
The study establishes patient-specific sequencing panels as a powerful tool for RMS management with several important clinical applications:
- Treatment response assessment without invasive procedures
- Early relapse detection before clinical symptoms or imaging changes
- Monitoring of treatment resistance and clonal evolution
- Personalized approach that accommodates tumor heterogeneity
This methodology represents a significant step toward truly personalized oncology, where monitoring strategies are tailored to each patient’s unique tumor genetics. As the technology becomes more accessible and cost-effective, it could transform how pediatric cancers are managed, reducing treatment morbidity while improving outcomes through earlier intervention.
The success of this tumor-informed approach in rhabdomyosarcoma suggests potential applications across other pediatric solid tumors where treatment response monitoring and early relapse detection remain significant clinical challenges. Future research will likely focus on standardizing these approaches and integrating them into routine clinical practice to maximize patient benefit.
Related Articles You May Find Interesting
- US-Australia Critical Minerals Partnership Counters China’s Supply Chain Dominan
- Elevance Health Defies Cost Pressures with $1.18 Billion Q3 Profit, Fueled by St
- Veteran Investor Launches $300M Digital Asset Fund After GoldenTree Spin-Out
- Voters in Colorado and Texas to Decide Divergent Tax Policy Measures This Novemb
- ST Telemedia’s Strategic Expansion in Maharashtra to Boost India’s Digital Infra
References & Further Reading
This article draws from multiple authoritative sources. For more information, please consult:
This article aggregates information from publicly available sources. All trademarks and copyrights belong to their respective owners.
Industrial Monitor Direct delivers unmatched 8 inch industrial pc solutions featuring fanless designs and aluminum alloy construction, endorsed by SCADA professionals.
Note: Featured image is for illustrative purposes only and does not represent any specific product, service, or entity mentioned in this article.